Beware the superbugs
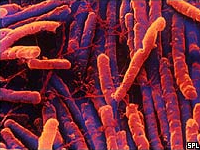
A survey carried out recently by CBC Marketplace in 54 Canadian hotels across six chains has revealed that potentially deadly antibiotic-resistant superbugs, including clostridium difficile and methicillin-resistant staphylococcus aureus were prevalent in guest rooms.
Results revealed varying levels of dirt and contamination but every hotel contained some form of antibiotic-resistant bacteria. The results were beamed across Canada on CBC television which had a fairly comprehensive effect on consumers and accommodation providers, as one could imagine.
Microbiologist Keith Warriner, who did the tests for Marketplace, singled out findings of clostridium difficile and staphylococcus aureus as alarming.
“It was a surprise at the start but amazing that all these hotels had superbugs,” he said. “When you get the antibiotic-resistant bacteria we’re finding, that’s not scare-mongering, that’s real. These are real pathogens that can cause real illnesses.”
Clostridium difficile is related to the bacterium that causes tetanus and botulism. It has two forms, an active, infectious form that cannot survive in the environment for prolonged periods and a non-active, “non-infectious” form, called a spore, that can survive in the environment for prolonged periods. Although spores cannot cause infection directly, when they are ingested they transform into the active, infectious form.
The highly virulent form, common in Europe and North America, has turned up in Australia.
This is a bug to take seriously. People can have post antibiotic diarrhoea and abdominal pain but, increasingly, it’s occurring in people who haven’t had antibiotics. And in a small percentage of people it can cause their death.
In the UK in 2005, an astounding one in 250 death certificates put down clostridium difficile as a contributing cause. It’s increased 50-fold in that country since 1990, and there are about 50,000 cases per year. What kills is often a major inflammation of the bowel that makes it dilate and perforate.
Clostridium difficile can be treated with antibiotics but in some people – particularly with hypervirulent forms – they can become “very, very sick very, very quickly”.
If we get clostridium difficile as badly in Australia as some overseas countries have it, it won’t be pretty.
About a third of the adult population carry (either on their skin or in their nose or mouth) bacteria called staphylococcus aureus. There are many different strains (types) of staphylococcus aureus (often referred to as staph or golden staph) and most of the time they live and multiply on the body without causing any problems. However, under some circumstances, they can get inside the body through broken skin and cause infection that requires treatment with antibiotics.
Some strains of staphylococcus aureus are difficult to treat as they have become resistant to commonly used antibiotics. Methicillin-resistant staphylococcus aureus has traditionally not been a problem for healthy people living in the community but was strongly linked with being in hospital. In recent years this picture has changed. Over the last few years new strains of methicillin-resistant have been identified which are known to spread and cause infection in healthy people living in the community and who have not been in hospital. These strains most commonly cause skin and soft tissue infections, however more serious infections can occasionally occur if staphylococcus aureus enters the bloodstream (from existing skin infection) or the lungs (following a respiratory illness). These infections can be life threatening.
The US Centers for Disease Control and Prevention report that staphylococcus aureus kills over 15,000 Americans each year, even more than AIDS. Staphylococcus aureus and other superbugs pose the greatest threat to those with weakened immune systems but can also be contracted through cuts or other open wounds.
While many people associate the drug-resistant germs with hospitals, Dr Warriner said he was surprised by the sheer prevalence of them in hotel rooms.
In Marketplace’s test, Dr Warriner examined 810 “high-touch” surfaces in rooms using an ultraviolet flashlight and an adenosine triphosphate meter that measures microbial contamination. Comforters proved the dirtiest, while faucets, remote controls, bed throws, bathroom sinks and toilet bases were the most commonly contaminated spots.
Hidden cameras in the rooms also captured maids using cleaning techniques that would actually help spread bacteria. One camera captured a maid using a toilet brush to clean a sink and another using same rag to wipe a toilet seat, then a faucet.
It is to be hoped that housekeeping staff can be made aware of these superbugs and assist in preventing the problem becoming as bad here as it is in North America and Europe.

AccomNews is not affiliated with any government agency, body or political party. We are an independently owned, family-operated magazine.





